Gardasil Fails to Protect Against Cervical Intraepithelial Neoplasia Over Time
Enthusiasm Over a Vaccine to Prevent Cervical Cancer Fades with Longitudinal Data
By Peter A. McCullough, MD, MPH
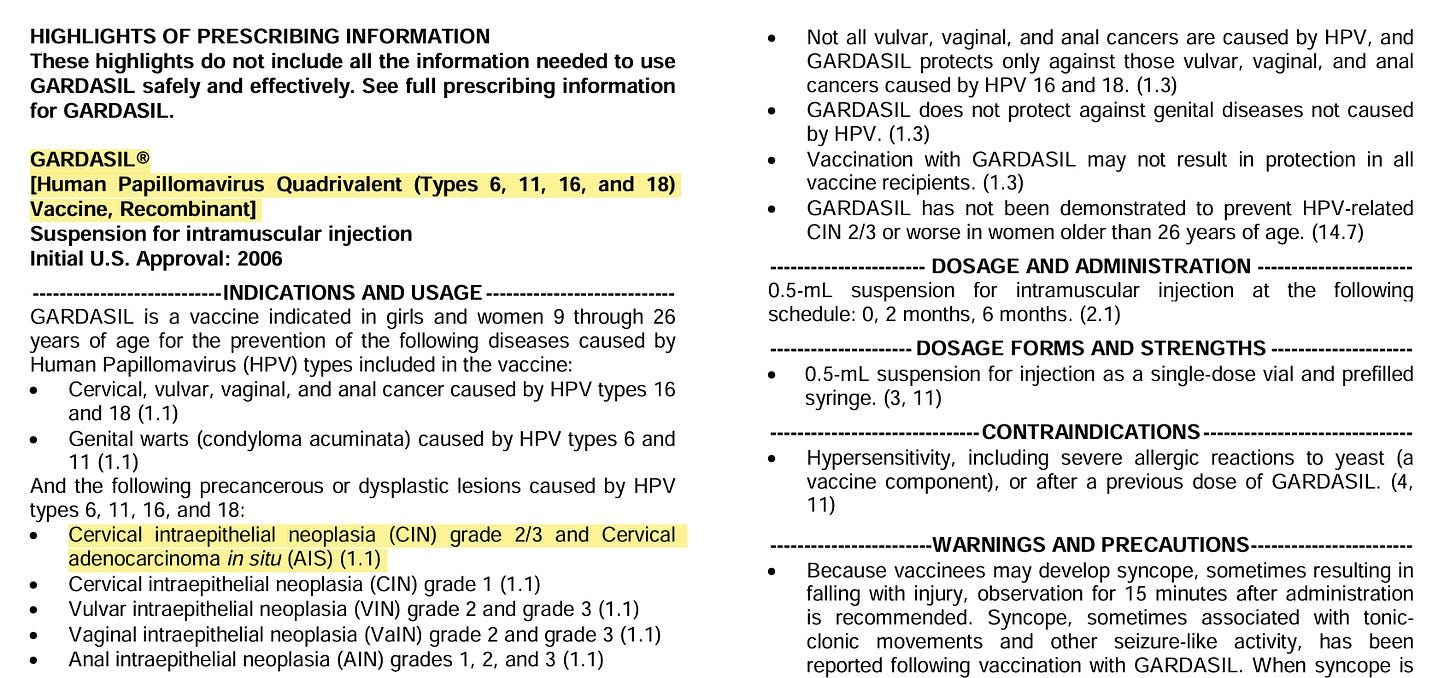
The US Food and Drug Administration (FDA) approved the first human papilloma virus (HPV) vaccine in 2006 progressing to Gardasil 9, a 9-valent vaccine, for use in children as young as 9 years old in December 2014. The CDC recommends the HPV vaccine as part of the routine vaccination schedule for children ages 11–12, but it can be given as early as age 9. The vaccine is also recommended for adults up to age 26, and in 2018 the FDA expanded the age range to include adults up to age 45.
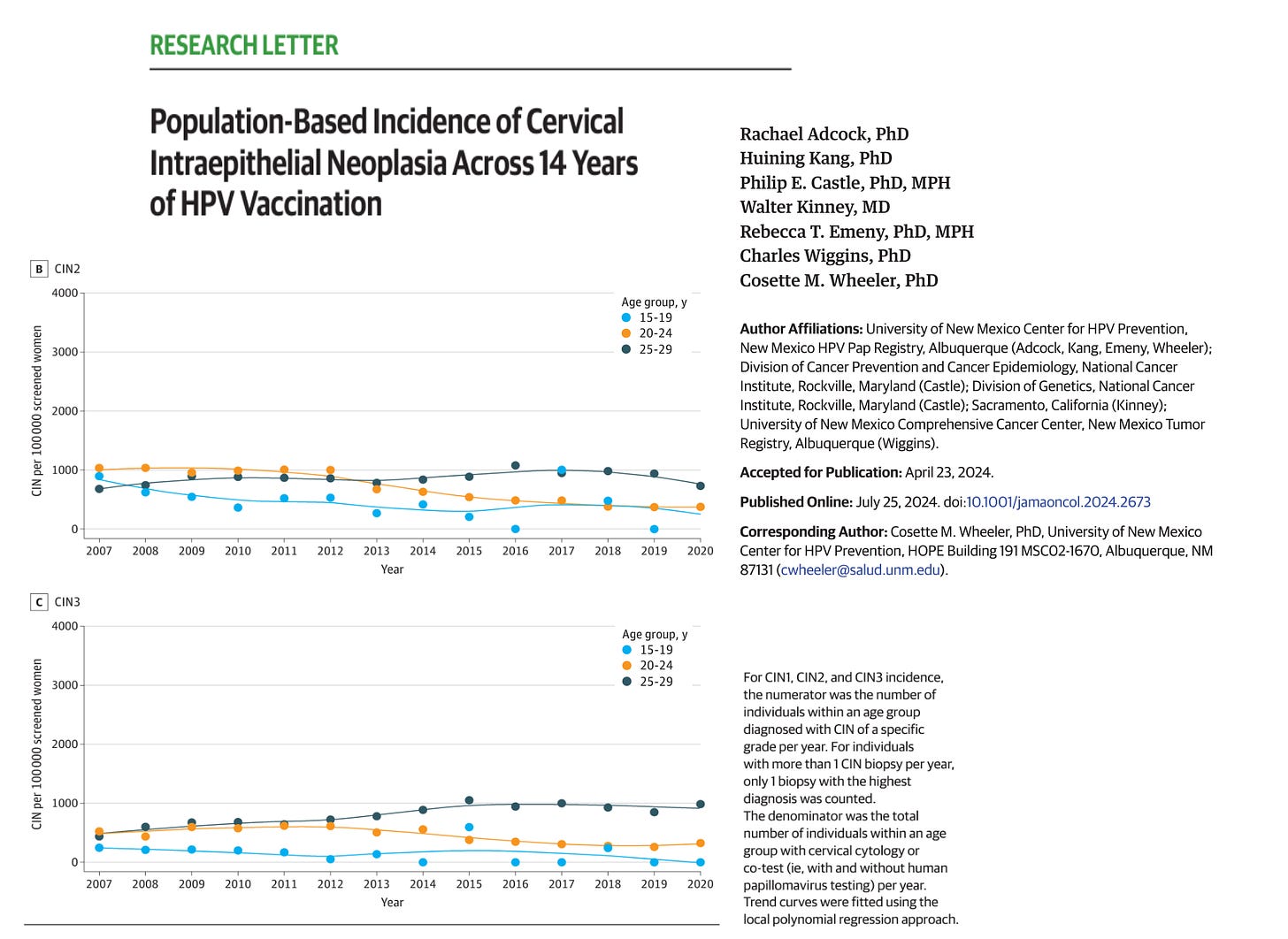
Adcock et al obtained data from January 1, 2007, to December 31, 2020, from the New Mexico HPV Pap Registry (NMHPVPR), the only comprehensive US statewide monitoring system for cervical cancer prevention. Over fourteen years through which the HPV vaccination should have had a population effect, the results are disappointing for the higher grades of cervical intraepithelial neoplasia 2 and 3, which are findings from a cervical biopsy that indicates abnormal cells on the cervix's surface. It's also known as high-grade or moderate dysplasia (CIN-2) and carcinoma in situ (CIN-3). CIN 2/3 is usually caused by infection with certain types of human papillomavirus (HPV).
The vaccine may be failing due to resistant strains, lack of compliance, or other reasons. It is possible that any favorable vaccine trend is overwhelmed by more intensive screening efforts. The main point for parents is not to be falsely reassured—HPV vaccination fails to protect against CIN-2 and CIN-3 on a population basis. So pelvic exams and PAP smears are necessary for sexually active teens and young women.
Please subscribe to Courageous Discourse as a paying ($5 monthly) or founder member so we can continue to bring you the truth.
Peter A. McCullough, MD, MPH
President, McCullough Foundation





I so regret giving this vaccine to my 3 daughters. Within a year and a half, one teen developed nausea similar to morning sickness and was eventually diagnosed with PCOS, one teen developed severe eczema. My last teen to get it has developed sleeping issues and mild eczema. None of these maladies run on either side of our families. Unnecessary suffering.
The article is behind a paywall, but by right clicking on the graphic above and opening it in a new window I can see some kind of decline for the rates of detection for 15 to 24 year olds.
There is no abstract, and the journal page lists none of the references. Fortunately, the PubMed page lists the references: https://pubmed.ncbi.nlm.nih.gov/39052303/ .
Since the rate of vaccination is increasing, if the vaccine was effective at preventing these neoplasms then the actual rate of incidence of these per 100k population would decrease, assuming (perhaps incorrectly) that the risk per person of being exposed to HPV and the risk of HPV infection leading to cancerous growths is stable over the study period. However, such a decrease might not be visible in the rate of detection if the rate of screening is also increasing. A quick look at the references made me think that they did not report population-wide screening rates or how this may have increased over the past decade or so.
It takes about ten seconds to type >> HPV "vitamin D" << into https://scholar.google.com and read the first result: ". . . women positive for HPV DNA found on the cervix and abnormal pap smear have significantly lower levels of serum vitamin D compared with women with negative HPV DNA . . .". This is Chu et al. 2021: https://journals.lww.com/jcma/fulltext/2021/11000/Vitamin_D_in_gynecological_diseases.12.aspx. The reference to "vitamin D" is to the circulating level of 25-hydroxyvitamin D, produced primarily in the liver, over several days, from UV-B produced or ingested vitamin D3 cholecalciferol.
This is not surprising to anyone who understands that the immune system needs at least 50 ng/mL 125 nmol/L circulating 25-hydroxyvitamin D to work properly, and that most people who do not supplement vitamin D3 properly (5 to 15 times the tiny quantities governments and many doctors recommend) and who have not had extensive UV-B (ideally white) skin exposure in the last few months typically have half or less of the required 50 ng/mL.
The Chu et al. data, from Taiwan, shows mean 25-hydroxyvitamin D levels of 22.04 ng/mL for women with no detected HPV, and 20.49 ng/mL for those with HPV detected. This is a marginal but statistically highly significant difference. This shows that the majority of these women have less than half of the 50 ng/mL 25-hydroxyvitamin D their immune systems need to function properly.
Here in Australia, at least one pathology lab has the reference range for 25-hydroxyvitamin D of 50 to 100 nmol/L, which is 20 to 40 ng/mL. So, according to this, if you have enough 25-hydroxyvitamin D for your immune system to work properly, the doctor will advise that your levels are toxic and that you should stop supplementing vitamin D3.
20 to perhaps 30 ng/mL is enough for the kidneys to play their part in regulating calcium-phosphate-bone metabolism, but most doctors and immunologists have no idea that the immune system needs at least 50 ng/mL to function properly. See: the graphs at the end of https://jamanetwork.com/journals/jamasurgery/fullarticle/1782085 or the two graphs combined at: https://vitamindstopscovid.info/00-evi/#00-50ngmL.
This 2014 article https://www.racgp.org.au/afp/2014/march/vitamin-d asks "If we can get all of the protective effect at 25(OH)D levels of 40–50 nmol/L, then why go higher?" So they think that 16 to 20 ng/mL is good for general health. The immune system is mentioned once, in passing.
Please read the research articles cited and discussed at: https://vitamindstopscovid.info/00-evi/ . This includes a tutorial on 25(OH)D to calcitriol intracrine and paracrine signaling and recommendations from Prof. Sunil Wimalawansa on how much vitamin D3 to supplement (according to body weight and obesity status) on order to safely attain at least the 50 ng/mL (125 nmol/L = 1 part in 20,000,000 by mass) level of circulating 25-hydroxyvitamin D the immune system needs to function properly. For average weight adults, this is about 0.125 milligrams = 5000 IU a day on average. This is a gram every 22 years. Pharma-grade vitamin D3 costs about USD$2.50 a gram ex-factory. There's very little vitamin D3 in food, fortified or not. UV-B exposure of ideally white skin can produce good amounts of vitamin D3, but this is not generally available all year round (high elevation sunlight on cloud-free days without intervening glass, clothing or sunscreen) and UV-B damages DNA and so raises the risk of skin cancer.
Many types of immune cell need a good level of 25-hydroxyvitamin D (produced mainly in the liver from ingested or UV-B-produced vitamin D3 cholecalciferol) in order to run their 25-hydroxyvitamin D to calcitriol intracrine and paracrine signaling systems. These work within a single cell (intracrine) and to nearby cells (paracrine). The conversion is activated by a cell-type specific condition and the resulting calcitriol changes the cell's behaviour in different ways for each cell type.