Influenza Vaccination Requirements for Health Care Personnel in US Hospitals
Acceptance Rates Dropping Despite Coercive Mandates
By Peter A. McCullough, MD, MPH
I counted 40 annual flu shots over the course of my life taken not for health reasons, but because I was required to do so during my education, training, and medical staff membership. I have never even suspected influenza in myself or my family members over six decades of life. Why the focus on influenza in healthy working age adults?
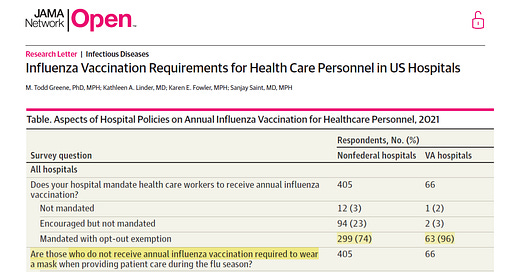
Greene et al surveyed nationwide practices for hospitals and health systems:
“The overall response rate was 48% (486 respondents from 1008 nonfederal and VA hospitals in the sample). Fifteen respondents (10 from nonfederal, 5 from VA) did not answer the influenza vaccination mandate question and were excluded, leaving 471 respondents (405 from nonfederal, 66 from VA) for the analysis. Questions about influenza vaccination policies for HCP are presented in the Table. Nonfederal hospitals reporting mandatory influenza vaccinations for HCP increased slightly but not significantly,2 from 69% (365 of 526) in 2017 to 74% (299 of 405) in 2021 (P = .14). In VA hospitals, mandatory influenza vaccinations increased significantly,2 from 4% (3 of 73) in 2017 to 96% (63 of 66) in 2021 (P < .001). Although mandating influenza vaccination for all HCP remains controversial, this study found a significant increase in VA hospitals requiring vaccinations for HCPs in recent years. Although there was a slight increase in mandates among nonfederal hospitals, mandates in VA hospitals increased substantially and are now nearly universal. This increase follows the implementation of Veterans Health Administration directive 1192.01 in August 2020, which explicitly required VA HCP to either receive influenza vaccination or obtain an exemption annually as a condition of employment.4 The findings demonstrate that many hospitals have made institutional commitments to increase vaccination coverage among HCP through mandates. While mandates are a strategy to increase vaccination rates among HCP, they may not be wholly effective in the COVID-19 era. Recent data showed that vaccination rates among HCP, which were increasing before the COVID-19 pandemic (89% in 2017-2018 to 91% in 2019-2020), have steadily decreased during the pandemic (86% in 2020-2021 to 81% in 2022-2023).5 Common vaccine hesitancy issues (eg, concerns about safety, mistrust of employers and authorities, and violation of personal autonomy) may have affected this shift.”
Keep reading with a 7-day free trial
Subscribe to Courageous Discourse™ with Dr. Peter McCullough & John Leake to keep reading this post and get 7 days of free access to the full post archives.