Long-COVID Associated with Elevated Antiviral Antibodies and Failed T-Cell Response
T-Cell "Exhaustion" May Explain Failure to Clear Spike Protein
By Peter A. McCullough, MD, MPH
Approximately 15% of patients after severe COVID-19 illness have long-COVID or post-acute sequelae including symptoms of fatigue, brain-fog, exercise intolerance, post-exertional malaise, neurological symptoms, etc. Why are only individuals affected?
A paper by Yin et al, performed a detailed proteomic and cellular analysis of a small group of patients with long-COVID to a group that had recovered after the illness.
“In summary, using multiple ‘omics’ analytical approaches, we found that long-COVID (LC) individuals exhibited phenotypic perturbations in both total and SARS-CoV-2-specific CD4+ and CD8+ T cells and changes in gene expression among CD4+ T cells, CD8+ T cells, monocytes and B cells. We found higher proportions of CD4+ TCM cells, TFH, cells and Treg cells in LC compared to recovered (R) individuals. SARS-CoV-2-specific CD8+ T cells, but not total CD8+ T cells, more frequently expressed the exhaustion markers PD1 and CTLA4, consistent with ongoing stimulation by viral antigens. Further supporting a potential persistent reservoir was our observation of higher SARS-CoV-2 antibody levels in LC individuals, consistent with reports of higher spike-specific IgG in LC compared to R individuals.”
The authors do not mention the vaccine status of the study subjects, likely those vaccinated had far worsened proteomic and cellular metrics given super-antigen loading with Spike protein that occurs with vaccination.
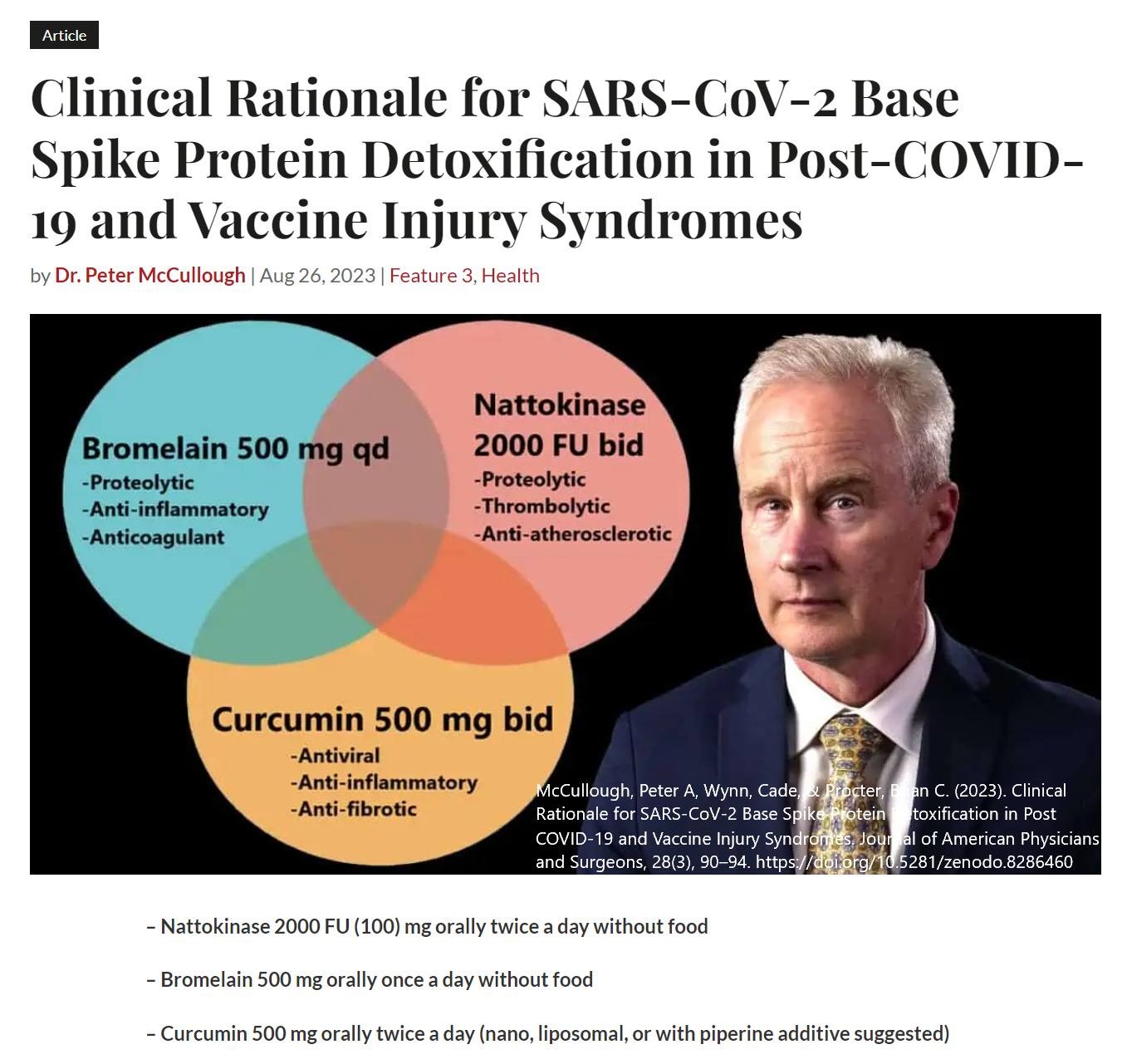
These data strongly support the Spike protein as the major driver of long-COVID syndrome. Thus, McCullough Protocol Base Spike Detoxification is a proposed cornerstone for treatment of post-acute sequelae after SARS-CoV-2 infection and vaccination. If the Spike protein is not handled, then all the other treatments are destined to provide only temporary relief of symptoms before they recur. We have found in our practice that Spike detoxification must fundamentally occur in the process of bona fide recovery.
Please subscribe to Courageous Discourse as a paying or founder member so we can continue to bring you the truth.
Peter A. McCullough, MD, MPH
President, McCullough Foundation




It is not surprising that so many people get sick and have long lasting symptoms from COVID-19. Most people have half or less of the 25-hydroxyvitamin D their immune systems need to function properly, at least in winter. Those with dark or black skin who live far from the equator have even lower 25-hydroxyvitamin D levels.
The ultraviolet B light which converts 7-dehydrocholesterol in the skin to vitamin D3 cholecalciferol also damages DNA and so raises the risk of skin cancer. If this was the only way of attaining vitamin D3 (only a few foods contain it, and then in extremely low quantities), then we would have to take the risk and use special lamps most of the year. Fortunately, vitamin D3 supplementation is inexpensive. It can be taken every 7 to 10 days.
For most people, the only practical way of attaining the 50 ng/mL (125 nmol/L) 25-hydroxyvitamin D we need is vitamin D3 supplementation in quantities well above the lousy 0.02 milligrams (800 IU) a day most governments recommend for adults. Neither vitamin D3 nor 25-hydroxyvitamin D (produced in the liver from vitamin D3) are hormones. (Vieth 2004 https://sci-hub.se/10.1016/j.jsbmb.2004.03.037.)
Please see the research on the vitamin D compounds and the immune system, cited and discussed at: https://vitamindstopscovid.info/00-evi/ .
https://vitamindstopscovid.info/00-evi/#00-how-much includes Prof. Sunil Wimalawansa's recommendations https://www.mdpi.com/2072-6643/14/14/2997 for vitamin D3 supplemental intake to attain at least the 50 ng/mL (125 nmol/L) circulating 25-hydroxyvitamin D, which the immune system needs to function properly. As he noted in a recent FLCCC webinar, these are ratios of body weight, with higher ratios for those suffering from obesity: https://odysee.com/@FrontlineCovid19CriticalCareAlliance:c/Weeekly_Webinar_Aug16_2023:d?t=3386 This is because people suffering from obesity convert less vitamin D3 into circulating 25-hydroxyvitamin D than normal-weight people.
The average daily vitamin D3 intake should be:
70 to 90 IU / kg body weight for those not suffering from obesity (BMI < 30).
100 to 130 IU / kg body weight for obesity I & II (BMI 30 to 39).
140 to 180 IU / kg body weight for obesity III (BMI > 39).
For 70 kg (154 lb) without obesity, this is about 0.125 milligrams (5000 IU) a day. This takes several months to attain the desired > 50 ng/mL circulating 25-hydroxyvitamin D. This is 6 or more times what most governments recommend. "5000 IU" sounds like a lot, but it is a gram every 22 years - and pharma grade vitamin D costs about USD$2.50 a gram ex-factory.
Vitamin D and dementia: https://vitamindstopscovid.info/00-evi/#3.3. The impact of low 25(OH)D on autism, preeclampsia, pre-term birth and low birth weight: https://vitamindstopscovid.info/00-evi/#3.2 .
Surely, proper 25-hydroxyvitamin D levels would help with long COVID.
Thank you Dr. McCullough! A True Truth Warrior who we so much Love and Appreciate!