McCullough Protocol©: Three Phases of Index COVID-19
Understanding Complex Illness is Key to Successful Therapy
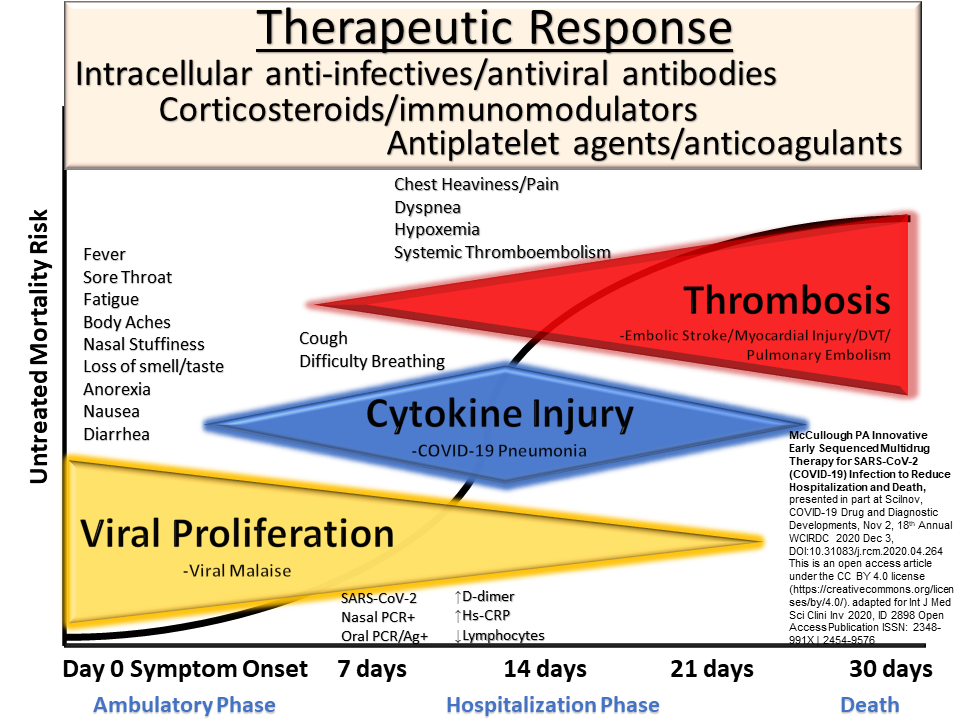
Coming up on three years of COVID-19 pandemic, clinicians have learned to appreciate the severity of illness that can occur in hospitalized patients. Grapsa, et al, published in JAMA on hospitalized patients from the Alpha to Omicron era in three Greek tertiary centers and found among survivors the hospital length of stay was 70 and 36.5 days for fully vaccinated and unvaccinated patients, respectively.[i] The 28-day mortality for those requiring mechanical ventilation was 61.5% and 68.2%, for fully vaccinated and unvaccinated patients, respectively. While confounding was not sufficiently handled to draw conclusions regarding vaccination and clinical outcomes, it is fair to say that both vaccinated and unvaccinated patients with severe COVID-19 have very high mortality and for the survivors, they must endure more than a month in the hospital. When McCullough et al, described three overlapping phases of COVID-19 illness in the “index” or first occurrence (viral replication, cytokine storm, and thrombosis) it allowed clinicians to approach the illness in a sequential manner and led to the understanding that a single drug would not provide comprehensive treatment for those at the highest risk of requiring hospitalization.
It is disappointing that none of the Infectious Disease Society of America (IDSA) or National Institutes of Health Guidelines (NIH) properly conceptualized the illness in this manner. As a result, the first NIH guideline in October of 2020, indicated that no treatment should be given to a patient in the ambulatory phase and only when hospitalized and requiring oxygen should the antiviral remdesivir be given as the initial therapy. For the average patient who has been ill at home for two weeks, one can see from the figure that the viral proliferation phase is nearly complete, and the patient is well into cytokine storm (inflammation) and pulmonary microthrombosis causing oxygen desaturation and respiratory distress. It is obvious from the figure it is far too late for remdesivir at that point and clinical priorities should be focused on supportive measures, anti-inflammatories, and anticoagulation. It should come as no surprise that in November, 2020, the World Health Organization advised against remdesivir for inpatient treatment of COVID-19.[ii] Sadly, the IDSA and NIH guidelines did not improve care and have been considered “not trustworthy” by the Academy of Critical Care: Development, Evaluation, and Methodology (ACCADEMY).[iii] Correct understanding of the multifaceted and phased natural history of COVID-19 led to the innovation of multi-drug therapy that begins ideally on day one of the illness and with the goal of shutting off the progression of disease to avoid hospitalization, mechanical ventilation, and death. When the debacle of government agency pandemic response is reviewed, likely this figure to appear and watch agency officials answer questions on why the U.S. featured the late use of remdesivir for inpatient treatment? Expect questions on why the agencies proposed the antiviral Paxlovid to work as monotherapy? Finally, there will be strong statements about how our government agencies failed to ask for “second opinions” from experts who were gaining insight on the phases of COVID-19 and matching successful therapy for patients in the community using multidrug regimens.[iv]
[i] Grapsa E, Adamos G, Andrianopoulos I, Tsolaki V, Giannakoulis VG, Karavidas N, Giannopoulou V, Sarri K, Mizi E, Gavrielatou E, Papathanakos G, Mantzarlis KD, Mastora Z, Magira E, Koulouras V, Kotanidou A, Siempos II. Association Between Vaccination Status and Mortality Among Intubated Patients With COVID-19-Related Acute Respiratory Distress Syndrome. JAMA Netw Open. 2022 Oct 3;5(10):e2235219. doi: 10.1001/jamanetworkopen.2022.35219. PMID: 36205996.
[ii] WHO recommends against the use of remdesivir in COVID-19 patients, Nov 20, 2020
[iii] Burns KEA, Laird M, Stevenson J, Honarmand K, Granton D, Kho ME, Cook D, Friedrich JO, Meade MO, Duffett M, Chaudhuri D, Liu K, D'Aragon F, Agarwal A, Adhikari NKJ, Noh H, Rochwerg B; Academy of Critical Care: Development, Evaluation, and Methodology (ACCADEMY). Adherence of Clinical Practice Guidelines for Pharmacologic Treatments of Hospitalized Patients With COVID-19 to Trustworthy Standards: A Systematic Review. JAMA Netw Open. 2021 Dec 1;4(12):e2136263. doi: 10.1001/jamanetworkopen.2021.36263. PMID: 34889948; PMCID: PMC8665373.
[iv] Procter BC, Ross C, Pickard V, Smith E, Hanson C, McCullough PA. Early Ambulatory Multidrug Therapy Reduces Hospitalization and Death in High-Risk Patients with SARS-CoV-2 (COVID-19). ijirms [Internet]. 2021Mar.17 [cited 2021Apr.28];6(03):219 - 221.




I used this excellent chart (among other protocols) to successfully treat a mild case of Omicron. Thank you Dr. McCullough for your prodigious and tireless work.