
COVID-19 Vaccination Looms as Larger Contributor to Myopericarditis Than SARS-CoV-2 Infection
Letter to the Editor reveals major bias in a recent JAMA study.
by Nicolas Hulscher, MPH
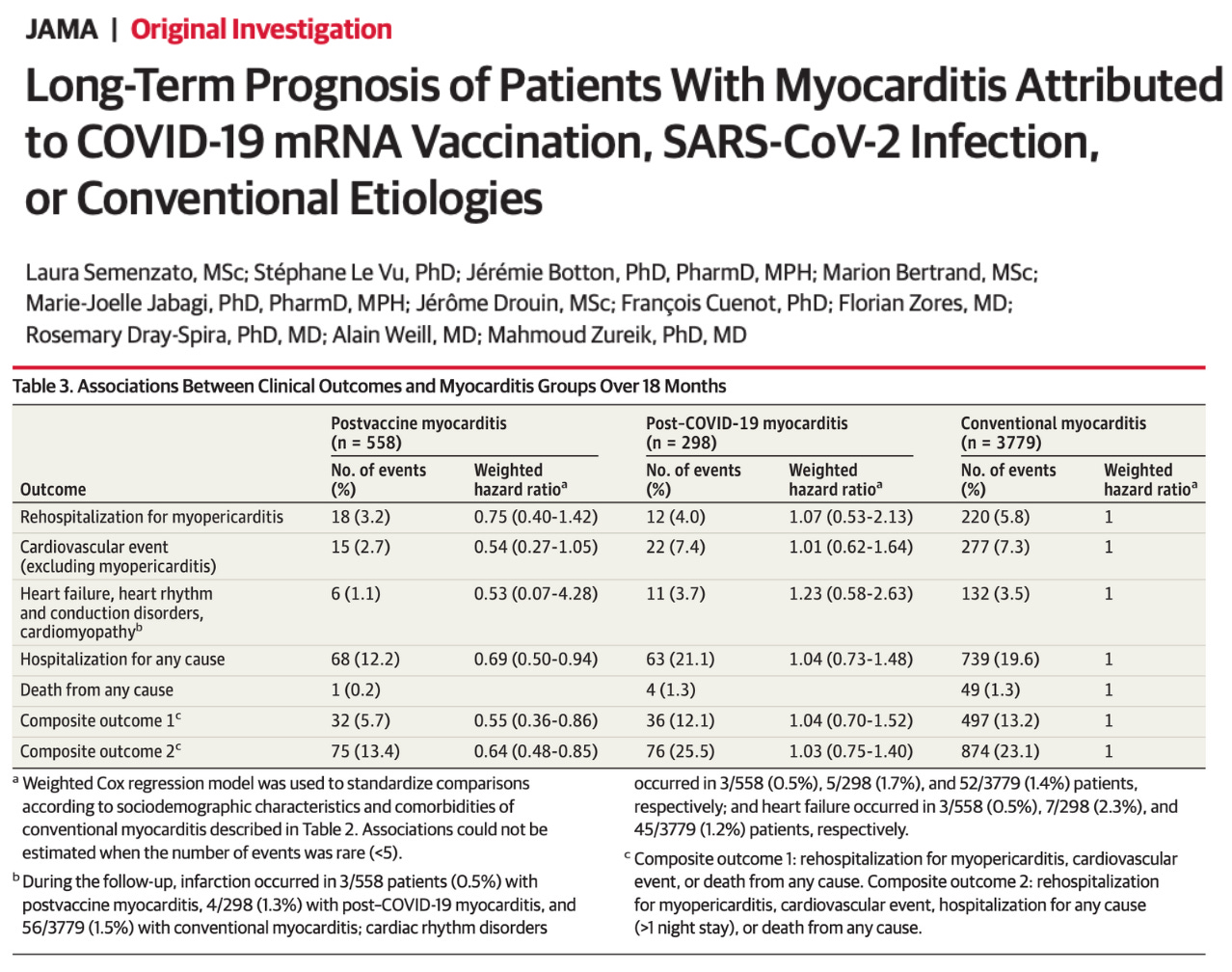
On August 26th, 2024, Semenzato et al published an article in JAMA claiming that patients who develop myocarditis following an mRNA COVID-19 vaccination experience fewer cardiovascular complications at 18 months compared to those with alleged myocarditis following a COVID-19 infection.
We identified major methodological flaws in their study that led to significantly biased conclusions. Thus, we (Nicolas Hulscher, MPH, Jessica Rose, PhD, and Peter McCullough, MD, MPH) submitted a Letter to the Editor to JAMA to highlight these concerns. Unfortunately, they declined to publish our research letter “because of the many submissions we receive and our space limitations in the Letters section.” We were fortunately able to publish our concerns in the non-partisan journal Science, Public Health Policy, and the Law: Letter to the Editor: Long-Term Prognosis of Patients with Myocarditis Attributed to COVID-19 mRNA Vaccination, SARS-CoV-2 Infection, or Conventional Etiologies:
Semenzato et al. incorrectly concluded that patients who develop myocarditis following an mRNA COVID-19 vaccination experience fewer cardiovascular complications at 18 months compared to those with alleged myocarditis following a COVID-19 infection or an unusually large series of those with “conventional” myocarditis allegedly not related to the infection or the vaccine [1]. The study methodology raises numerous concerns. According to Table 2, among the post-COVID-19 myocarditis and ‘conventional’ myocarditis groups, 46.3% and 52.3% received at least one COVID-19 vaccine, respectively. Since Semenzato et al. did not incorporate a proper clinical adjudication protocol for myocarditis, it is likely that a substantial number of patients in the post-COVID-19 and ‘conventional’ groups actually had cardiovascular conditions and laboratory results that triggered automated codes mapping to myocarditis. For example, elevated troponin values commonly found with hospitalized illness do not alone indicate myocarditis. Moreover, vaccine-induced myocarditis was defined as patients diagnosed with myocarditis within 7 days of inoculation, while post-COVID-19 myocarditis was given a 30-day window since the initial infection. The authors cite Le Vu et al. as justification for this methodological choice [2], where 331 hospitalized cases experienced myocarditis or pericarditis from 8 to 21 days following vaccination and were not classified as “post-vaccination cases” because they didn’t occur within 7 days. The 7-day vaccine myocarditis window is obviously biased and may be approximately four times more likely to ascribe myocarditis to the infection as opposed to the vaccine. After COVID-19 vaccination, the mRNA has been found in blood 28 days after injection [3] and the vaccine-derived prefusion stabilized Spike protein is circulatory in blood for at least six months [4], suggesting there is a very large window after vaccination where myocarditis is a plausible vaccine injury syndrome.
For our response, Dr. Jessica Rose queried the the Vaccine Adverse Event Reporting System (VAERS) to investigate the percentage of vaccine-induced myocarditis that occurs after the 7-day window employed by Semenzato et al:
The number of reports that occurred more than 7 days post injection was 4,602. 32.4% of myocarditis/myopericarditis cases were reported more than 7 days after the last vaccination, meaning that 67.6% of reports qualify as “vaccine-induced myocarditis” according to the definition provided by Semenzato et al. [1]. Notably, among these reported post-injection myocarditis cases more than 7 days after injection, 67.5% were listed as “not recovered” at the time of the report, of which the mean age was 35. These data indicate that Semenzato et al’s choice of post-vaccine myocarditis limited to 7 days after injection was biased and worked to falsely reduce cases of myocarditis attributed to vaccination. The authors do partially acknowledge this limitation in eTable4, where they redefine cases of post-vaccine myocarditis as having received an mRNA vaccine within the previous 30 days instead of 7 days. This more balanced analysis resulted in a higher weighted hazard ratio (wHR) for the composite outcome in post-vaccine myocarditis cases (wHR = 0.84) compared to the original analysis (wHR = 0.55), which would significantly alter Semenzato et al.’s conclusions.
The conclusions made by Semenzato et al are also not consistent with the literature:
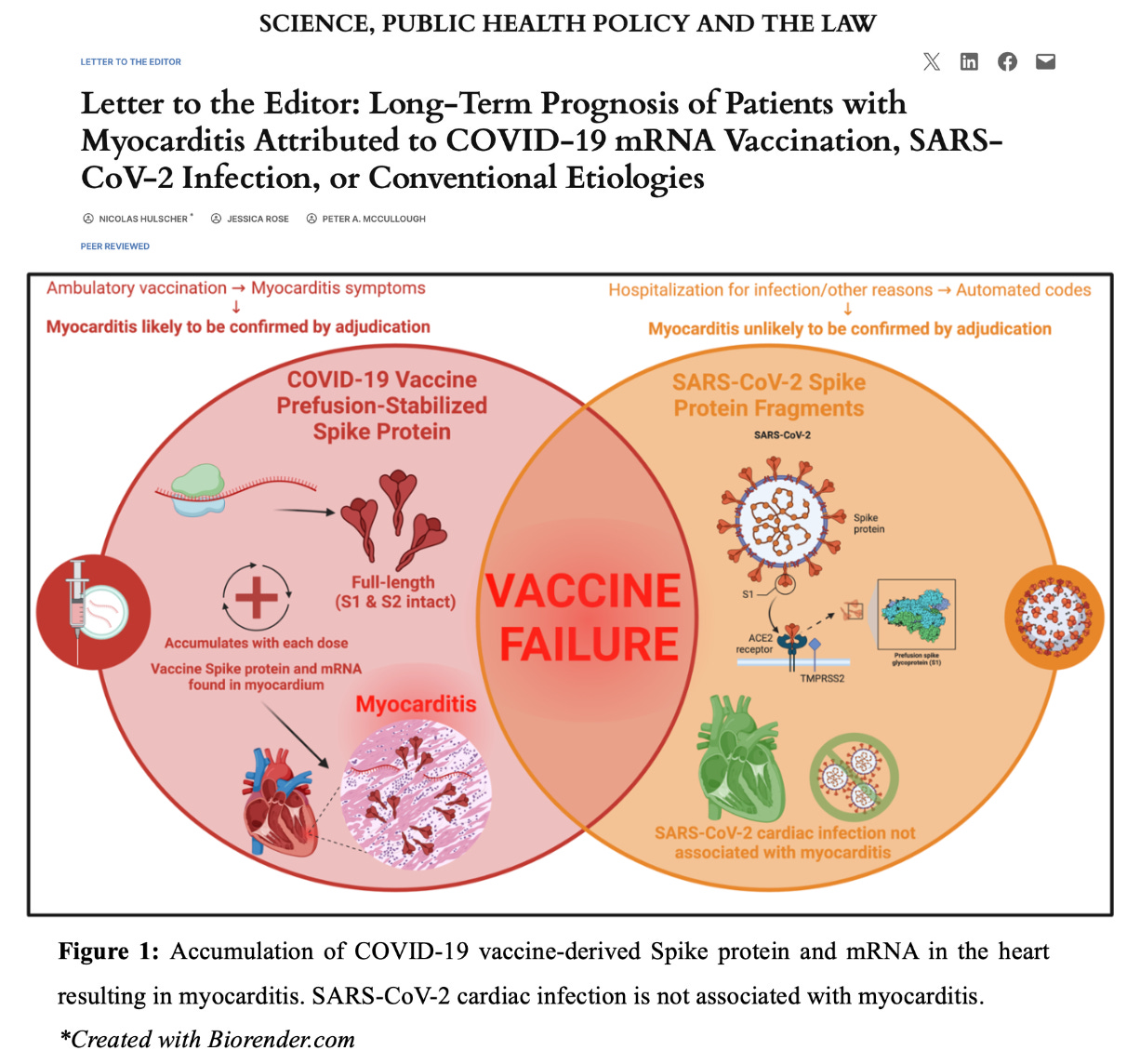
Watanabe and Hama found that the myocarditis mortality rate ratio (MMRR) was significantly higher in the COVID-19 vaccinated population compared to the general population during the three years preceding the COVID-19 pandemic, with a pronounced increase among young adults (MMRR: 7.80 for individuals in their 30s) [6]. The OpenSAFELY study found that myocarditis occurred only among COVID-19 vaccinated children and not SARS-CoV-2 infected children, with a sample size of over 1 million participants [7]. Both mRNA and vaccine-derived Spike protein with inflammation have been found in the human heart in those who died after COVID-19 vaccination and in those with vaccine-induced myocarditis, respectively (Figure 1) [8, 9]. Whereas autopsies of individuals who died from SARS-CoV-2 infection indicate that cardiac infection with the virus is not associated with myocarditis [10].
And finally, our conclusion:
In conclusion, the study by Semenzato et al. is misleading. SARS-CoV-2 infection does not cause serious myocarditis [7, 10], whereas COVID-19 vaccination is well recognized to cause symptomatic and fatal myocarditis [6, 11]. Future prospective cohort studies should classify patients correctly, have extended and equal windows of observation, and clinical adjudication with exam, ECG, blood biomarkers, and cardiac imaging. The use of automated data sources alone should not be relied upon for comparative studies because it is subject to investigator bias and is greatly misleading.
Nicolas Hulscher, MPH
Epidemiologist and Foundation Administrator, McCullough Foundation
www.mcculloughfnd.org
Please consider following the McCullough Foundation and Nicolas Hulscher on X (formerly Twitter) for further content.
References
1) Semenzato L, Le Vu S, Botton J, et al. Long-Term Prognosis of Patients With Myocarditis Attributed to COVID-19 mRNA Vaccination, SARS-CoV-2 Infection, or Conventional Etiologies. JAMA. Published online August 26, 2024. doi:10.1001/jama.2024.16380
2) Le Vu S, Bertrand M, Jabagi MJ, et al. Age and sex-specific risks of myocarditis and pericarditis following Covid-19 messenger RNA vaccines. Nat Commun. 2022;13(1):3633. Published 2022 Jun 25. doi:10.1038/s41467-022-31401-5
3) Castruita JAS, Schneider UV, Mollerup S, et al. SARS-CoV-2 spike mRNA vaccine sequences circulate in blood up to 28 days after COVID-19 vaccination. APMIS. 2023;131(3):128-132. doi:10.1111/apm.13294
4) Brogna C, Cristoni S, Marino G, et al. Detection of recombinant Spike protein in the blood of individuals vaccinated against SARS-CoV-2: Possible molecular mechanisms. Proteomics Clin Appl. 2023;17(6):e2300048. doi:10.1002/prca.202300048
5) U.S. Department of Health and Human Services. Vaccine adverse event reporting system (VAERS) [Internet], https://vaers.hhs.gov (2024, Accessed 27 August 2024).
6) Watanabe S, Hama R. SARS-CoV-2 vaccine and increased myocarditis mortality risk: A population based comparative study in Japan. medRxiv. 2022. DOI: 10.1101/2022.10.13.22281036.
7) Andrews CD, Parker EPK, Horne E, Walker V, Palmer T, Schaffer AL, et al. OpenSAFELY: Effectiveness of COVID-19 vaccination in children and adolescents. medRxiv. 2024; DOI: 10.1101/2024.05.20.24306810
8) Krauson AJ, Casimero FVC, Siddiquee Z, Stone JR. Duration of SARS-CoV-2 mRNA vaccine persistence and factors associated with cardiac involvement in recently vaccinated patients. NPJ Vaccines. 2023;8(1):141. Published 2023 Sep 27. doi:10.1038/s41541-023-00742-7
9) Baumeier C, Aleshcheva G, Harms D, et al. Intramyocardial Inflammation after COVID-19 Vaccination: An Endomyocardial Biopsy-Proven Case Series. Int J Mol Sci. 2022;23(13):6940. Published 2022 Jun 22. doi:10.3390/ijms23136940
10) Lindner D, Fitzek A, Bräuninger H, et al. Association of Cardiac Infection With SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases. JAMA Cardiol. 2020;5(11):1281-1285. doi:10.1001/jamacardio.2020.3551
11) Hulscher N, Hodkinson R, Makis W, McCullough PA. Autopsy findings in cases of fatal COVID-19 vaccine-induced myocarditis. ESC Heart Fail. Published online January 14, 2024. doi:10.1002/ehf2.14680









Thank you for your publication. It is unscientific to not accept your work.
Looks like JAMA is "off the rotation"!
When I read the paper a couple of weeks ago, it was obvious when they used a 7 day window for the post vaccine-induced myocarditis, and a 30 day window for the post Covid myocarditis, that the paper was a fraud. I continue to find it stunning that reviewers (if the paper was even sent out for review) and the editor of the JAMA would stoop to this level of misrepresentation, flawed study design, and false conclusions.