SARS-CoV-2 Infection Causes Dysregulation of Proteome in Long-COVID for 18 Months or Longer
POTS Manifested by Heart Pounding and Passing Out in Long-COVID May Have Fundamental Proteomic Underpinnings
By Peter A. McCullough, MD, MPH
I have been impressed with the large numbers of people on camera and in public who experience heart pounding dizziness and at times completely pass out. This syndrome is called Postural Orthostatic Tachycardia syndrome (POTS) and is manifested by the heart rate increasing very quickly after getting up from sitting or lying down. In extreme cases it causes dizziness and near syncope or syncope. POTS occurs after both SARS-CoV-2 infection and ill-advised COVID-19 vaccination.
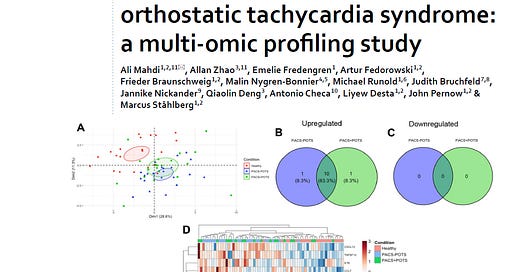
Mahdi et al performed a detailed analysis of twenty-one healthy control subjects without a prior COVID-19 infection (mean age 43 years, 95% females), 20 non-hospitalized patients with post-COVID-19 acute sequelae (PACS) otherwise known as long-COVID with POTS (mean age 39 years, 95% females) and 22 non-hospitalized patients with PACS but without POTS (mean age 44 years, 100% females). Post-COVID patients were studied ~18 months the the infection. Cardiometabolic proteomic analyses revealed a dysregulation of ≈200 out of 700 analyzed proteins in both PACS groups vs. healthy subjects with the majority (> 90%) being upregulated. There was a large overlap (> 90%) with no major differences between the PACS groups. Gene ontology enrichment analysis revealed alterations in hemostasis/coagulation, metabolism, immune responses, and angiogenesis in PACS vs. healthy controls. Furthermore, 11 out of 33 cytokines/chemokines were significantly upregulated both in PACS + POTS and PACS-POTS vs. healthy controls and none of the cytokines were downregulated. There were no differences in between the PACS groups in the cytokine levels. Lastly, 16 and 19 out of 88 sphingolipids were significantly dysregulated in PACS + POTS and PACS-POTS, respectively, compared to controls with no differences between the groups. Here are the authors conclusions:
“Patients with PACS demonstrate distinctly altered plasma protein, cytokine and lipid profiles compared with healthy controls. In particular, alterations in hemostasis, T-cell proliferation, apoptosis and amino acid metabolism may be potentially involved in symptom development and maintenance in PACS. Interestingly, plasma profile of PACS patients with and without POTS do not substantially differ, implying that PACS is associated with alterations in plasma profile regardless of POTS presence. Other pathophysiological mechanisms may be responsible for the development of POTS in PACS. Collectively our data suggest that the pro-inflammatory/proliferative and pro-coagulative state in PACS represents an important phenotype in the pathophysiology of the disease and might largely explain the disease burden of the population. This may lay the foundation for future clinical investigations with focus on inflammation resolution, resolution of micro clots and rearrange the hemostasis to alleviate the disease burden or dissect possible biomarkers for disease progression in PACS.”
Keep reading with a 7-day free trial
Subscribe to Courageous Discourse™ with Dr. Peter McCullough & John Leake to keep reading this post and get 7 days of free access to the full post archives.