Similar In-Hospital and 30-day Outcomes for Omicron and Influenza
No Observable Benefit of Vaccination Campaigns in the Elderly
By Peter A. McCullough, MD, MPH
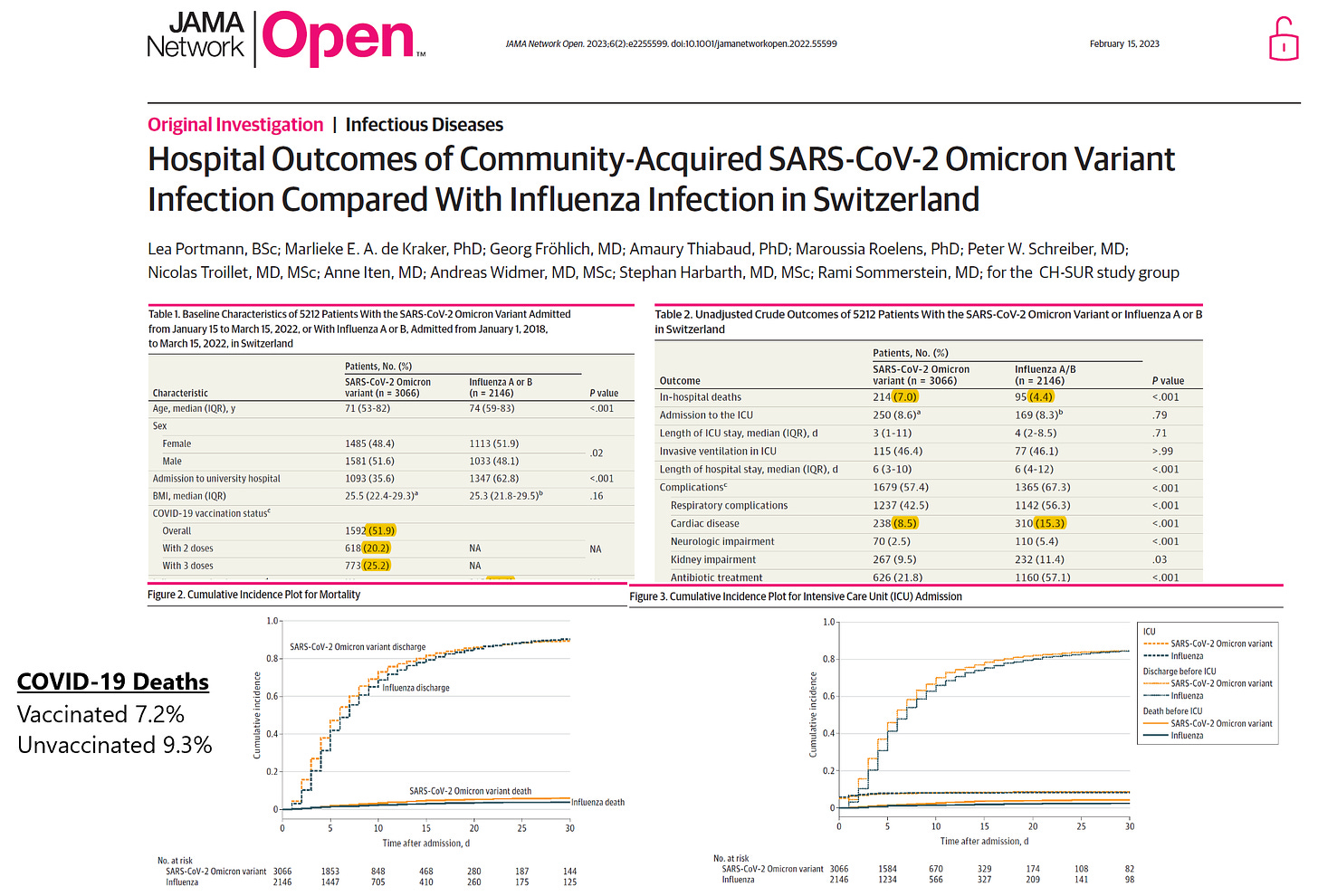
Clinical concerns over both COVID-19 and influenza should have remained on the vulnerable elderly population, particularly those in senior centers. Instead we have seen a two-year media blitz on vaccinating young healthy working age persons and children. Portmann and colleagues published a sobering report on hospitalized cases of Omicron and Influenza A/B infections in Switzerland. The in-hospital mortality rates were 7.0 and 4.4% with 8.5 and 15.3% incurring cardiovascular events in the SARS-CoV-2 and Influenza A/B groups, respectively. This translated into nearly identical outcomes (ICU admission and death) at 30 days in both groups. There appeared to be no impact of antecedent vaccination for either disease but for different reasons. The COVID-19 vaccinations failed to stop hospitalization with the majority having been immunized. There was no statistical difference in death among those vaccinated verses not, 7.2 vs 9.3%, p=0.05, respectively. Influenza vaccination appeared to have no impact because of very poor utilization (10%) with considerable missing data.
Portmann failed to report on the most important variable in both conditions—prehospital care. Use of early multidrug therapy and home/senior center care are the only interventions that can reduce the risk of hospitalization and death. We cannot rely on vaccination to help in our seniors and must shift the focus to care in the prehospital phase of respiratory illness.
If you find “Courageous Discourse” enjoyable and useful to your endeavors, please subscribe as a paying or founder member to support our efforts in helping you engage in these discussions with family, friends, and your extended circles.





Thank you for continuing to mention early treatment every chance you get. You're almost alone in this endeavor, and as far as I can tell, it is the SINGLE MOST IMPORTANT issue at hand. How many hundreds of thousands, perhaps millions of lives could've been saved with appropriate early treatment? And still, almost no one even mentions it. Thank you again, Dr. McCullough.
The best research shows that influenza vaccines do not reduce the risk of hospitalisation or death for influenza or for respiratory infections in general. See Anderson et al. 2020 https://sci-hub.ru/10.7326/M19-3075 and my two articles discussing this and related research: https://nutritionmatters.substack.com/p/influenza-vaccines-do-not-reduce
The COVID-19 pandemic response has been a cluster of crimes against humanity, regarding the suppression of vitamin D3 and other nutrients and of inexpensive early treatments, the problems caused by the quasi-vaccines, the lockdowns, social distancing, masks etc. https://nutritionmatters.substack.com/p/the-covid-19-pandemic-response-killed .
Please see the most important research on vitamin D and the immune system, cited and discussed at my long page (co-signed by Patrick Chambers MD): https://vitamindstopscovid.info/00-evi/ .
It is abundantly clear that we must get everyone's 25-hydroxyvitamin D (25(OH)D) levels up to the 50 ng/mL 125 nmol/L level their immune system needs to function properly. The above page has recommendations from Prof. Sunil Wimalawansa on how to attain this in the long term with vitamin D3 supplemental quantities as ratios of body weight, with higher ratios for those suffering from obesity. This is from his article: https://www.mdpi.com/2072-6643/14/14/2997 . The ratios are in a table at: https://vitamindstopscovid.info/00-evi/#sjw-updated-ratios . See the section before this for the mechanisms which cause the need for higher ratios for those suffering from obesity. These do not apply to normal weight or overweight people. I argue that there is no observational or mechanistic justification for the lower ratios recommended by Prof. Wimalawansa for underweight people. For 70kg 154 lb body weight without obesity, 0.125 mg (5000 IU) a day will get most people's 25(OH)D level safely over 50 ng/mL, over several months. This is a gram every 22 years - and pharma grade vitamin D3 costs about USD$2.50 a gram.
Bolus (10 mg, 400,000 IU) vitamin D3 takes about 4 days to raise 25(OH)D levels safely over 50 ng/mL, from typical unsupplemented levels of 5 to 25 ng/mL. The delay is due to the need for hydroxylation in the liver.
For all clinical emergencies, such as sepsis, COVID-19, Kawasaki disease, MIS-C etc. the most urgently needed treatment for most people is to boost their 25(OH)D level safely over 50 ng/mL in about 4 hours. This can only be done with oral calcifediol - which _is_ 25-hydroxyvitamin D. As Prof. Wimalawansa recommends, 0.014 mg per kg bodyweight will reliably and very safely achieve this in all people, no matter how low their 25(OH)D level was. See his article and: https://nutritionmatters.substack.com/p/calcifediol-to-boost-25-hydroxyvitamin . This is the most important treatment for all those suffering from severe influenza, COVID-19, sepsis etc. However, the most important step is to prevent all this suffering, harm and death by proper vitamin D3 supplementation in the long term.