Allergies have surged significantly over the past decades, becoming a critical public health concern worldwide. This rise represents a shift from viewing allergies as a seasonal nuisance to understanding their public health implications and how they serve as an indicator of the overall health of the global population.
To fully grasp the current allergy epidemic, it’s essential to understand how scientific perspectives on this disease have changed over time. We must look back at how our understanding of allergies has evolved and how this reflects in our modern health landscape.
Austrian pediatrician Clemens Von Pirquet first pioneered the term “allergy” in 1906. While examining reactions to vaccine inoculations—symptoms like fever, rashes, and joint pain—Pirquet noted what he called “serum disease” or “serum sickness.” Pirquet then proposed that these reactions were the result of antigen-antibody complexes forming in the body, introducing the idea of immune reactivity to external agents as a distinct phenomenon. This concept set the stage for our modern understanding of allergies as immune responses that can become excessive or misguided.
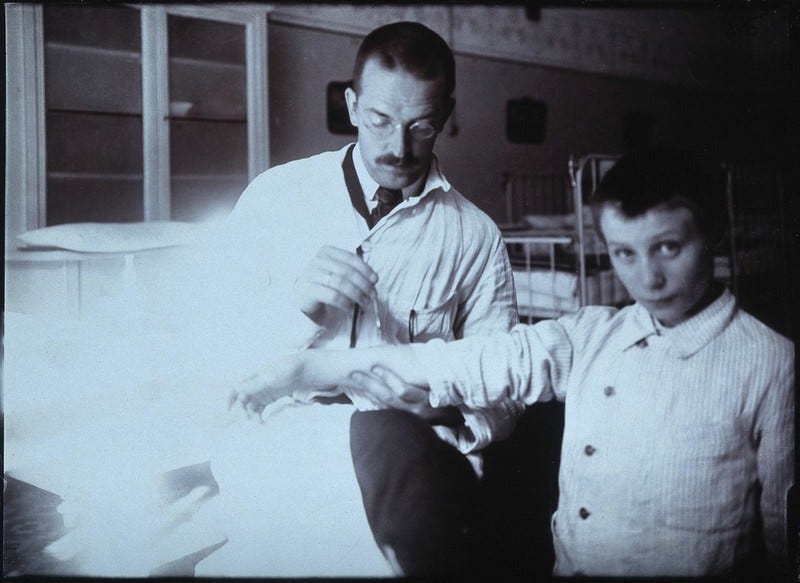
In the years following Pirquet’s discovery, American pediatrician Oscar Schloss authored a research report in which he described a revolutionary diagnostic method for allergy detection through a skin scratch test. Subsequently, American immunologist Robert Cooke suggested the mechanism to “desensitize” or “hyposensitize” patients who demonstrated sensitivity to certain allergens. These findings led to the introduction of allergen immunotherapy treatments now utilized globally by allergists, including myself, to effectively treat this ailment.
These early pioneers broadened the scientific understanding of allergy and the complexity of immunological responses.
According to 2021 CDC data, an estimated 1 in 4 U.S. adults and 1 in 3 U.S. children have at least one allergy, whether it’s seasonal, eczema, or food-related. This statistic highlights allergies as a significant public health issue with wide-reaching effects.
Research also suggests that allergies can impact children’s academic performance. A study from Spain found that allergies—particularly allergic rhinitis—can cause substantial sleep disturbances, which in turn lead to increased school absenteeism and diminished academic performance. Notably, they find that treatment through second-generation antihistamines is shown to mitigate the affected school performance in this population of pediatric patients.
Other research from the IMMUNOe Research Centers in Colorado, for example, demonstrates an intriguing link between allergic rhinitis and ADHD. They propose that allergic rhinitis can “trigger an immune inflammatory cascade that may lead to the neuroimmune inflammation presented clinically as ADHD.” Interestingly, their findings showed improvements in “ADHD scores” in patients treated for allergic inflammation, suggesting a complex interaction between allergic disease and other inflammatory processes.
I had the privilege of conducting research alongside my late mentor, the esteemed Dr. Lyndon Mansfield—a legend in the field of Allergy and Immunology. Together, we conducted a double-blind, placebo-controlled study known as TOVA (Tests of Variables of Attention). In this trial, we demonstrated that children misdiagnosed with ADHD showed significant improvements in symptoms when treated with anti-allergic medications. This finding highlights the importance of accurate diagnosis and the potential for allergic interventions to impact broader neuroimmune functions.
This data underscores the largely overlooked issue of allergies as a serious global health issue. In my recent article, I discussed the broader trend of rising non-communicable diseases (NCDs) worldwide, with allergies as a notable contributor. Allergic conditions, when persistent and untreated, can lead to a cascade of inflammatory responses, contributing to the global epidemic of NCDs.
Last month, I had the opportunity to address this topic at the Expo Pharma Summit 2024 in Guadalajara, Mexico. During my talk, I emphasized how the growing incidence of allergies is already shaping the pharmaceutical industry. I presented data showing that this increase will significantly impact pharmaceutical demand in the years ahead. For instance, antihistamines, which remain the primary treatment for environmental allergies, are expected to see their market size more than double over the next 8 to 10 years.

What is the reason behind this rise?
It seems there are various theories, one that has taken prevalence recently is that of the hygiene hypothesis. Originally coined by Epidemiologist David Strachan, who found how early childhood exposure to infectious agents via unhygienic practices within a household, led to a lower incidence of eczema and other allergic reactions within those patients.
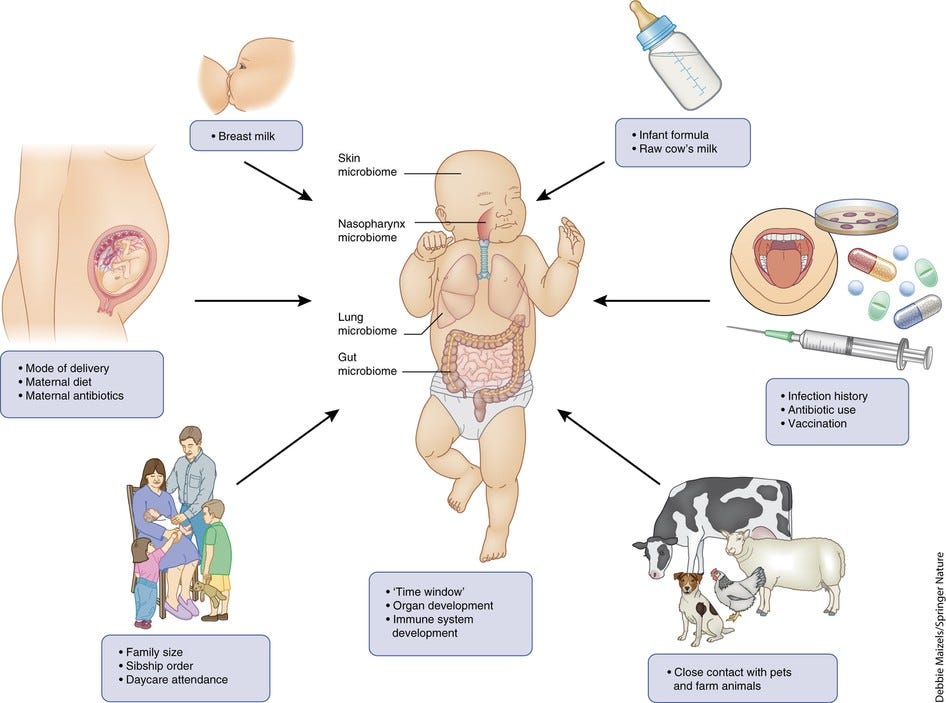
The hygiene hypothesis has since expanded to encompass broader inflammatory diseases, suggesting that our “sanitized” environments, arising from the rapid industrialization of the last 100 years, may hinder the immune system’s natural training processes. Without regular exposure to a range of microorganisms, our immune system may respond disproportionately to benign substances, contributing to chronic inflammation and immune dysregulation.
There are, however, additional factors to consider. In my conference, I discussed the possible influence of environmental shifts as contributing to the rise in allergies. Factors such as prolonged pollen seasons, increased allergenicity of pollens, and heightened exposure to pollutants all create conditions that may exacerbate allergic reactions and lead to a greater prevalence of allergies globally.
For these reasons, I emphasize the importance of an immunological perspective when addressing the chronic health crises of our time. The research cited, such as the ADHD and allergic rhinitis studies, highlights a clear link between allergic inflammation and broader immune function. These findings show how allergic diseases not only impact specific symptoms but also connect to other systemic and neuroimmune responses, contributing to a cascade of chronic health conditions.
The COVID Operation era lockdown policies characterized by widespread isolation and reduced microbial exposure, contributed to broad immunosuppression. These conditions weakened immune responses across the population, leading to a significant increase in allergic diseases. This amplification of immune dysregulation, spurred by reduced natural exposures, underscores how seemingly isolated immune responses, such as those seen in allergies, may contribute to the broader epidemic of chronic inflammatory diseases.
As allergies become more widespread, their role in influencing other inflammatory, non-communicable diseases (NCDs) is becoming clearer. Once seen as a seasonal annoyance, allergies now represent a genuine public health concern with potential links to conditions such as asthma, autoimmune disorders, and even metabolic diseases. Addressing this issue will require a public health approach that considers the complex interactions between immunity, environmental factors, and lifestyle.
This brings me to my core, underlying message. To tackle the chronic disease epidemic effectively, we must address the root causes of these conditions. Confronting these issues demands a true shift toward a more functional and holistic approach to health—one that considers the full spectrum of factors impacting the immune system and overall wellness. Only by addressing these underlying drivers can we make meaningful strides in reducing the burden of chronic, non-communicable diseases.
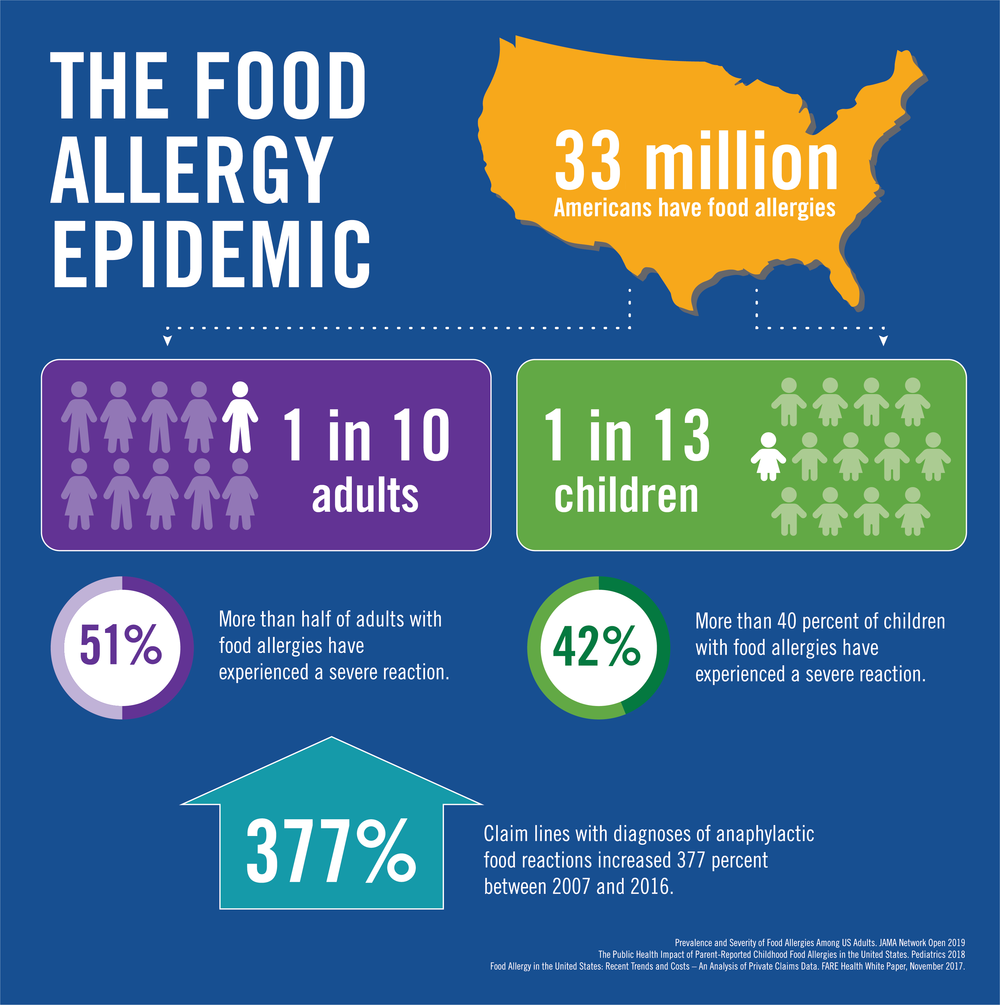
I have yet to fully address the impact of food in this ongoing health crisis. According to recent data, 1 in 13 children and 1 in 10 adults in the United States now suffer from food allergies, a dramatic increase over the past few decades. This rise is particularly evident in the last 20 years, with studies suggesting a strong correlation between environmental factors, changes in diet, and increased exposure to food additives. These developments highlight the urgent need for a reevaluation of food safety and its role in the current public health challenges.
In a recent video, Robert F. Kennedy Jr. discussed the impact of food additives on not just allergies, but overall health. He specifically highlighted tartrazine, or yellow dye #5, which is commonly used in junk food by major manufacturers. Kennedy explained that this chemical was originally derived from the sludge left over after turning coal into coke. British chemists later discovered its potential as a food coloring agent. Initially introduced to enhance the appearance of low-quality food, tartrazine is now widely present in everyday food products, and even in medications. This is just one example of how food additives are contributing to the rise in food allergies and broader health concerns.
These products that are on “every supermarket shelf”, as Kennedy mentions, are some of the leading drivers of this chronic health epidemic. They are making children more asthmatic, anxious, depressed, and more susceptible to developing autoimmune disorders.
Health consciousness is shifting. In recent years, particularly after the pandemic era, people have become more aware of the tragic mistakes that have been committed in the handling of public health over the last decades. Movements such as the 'Make America Healthy Again' (MAHA) initiative, which following recent electoral results in the United States, is now set to reshape the country’s health regulatory agencies. There is undoubtedly an increasing relevance to the issue of Biopolitikal policy. This growing awareness is influencing health policy in the highest spheres of global politics. It is widely understood, that whatever the United States does, the world will follow. For that reason, I think we should pay close attention to how the MAHA agenda will shape health policy not just in the United States but worldwide.
“My spirit shall not abide in man for ever, for he is flesh; his days shall be a hundred and twenty years.” (Genesis 6:3)
FIN
Biopolitiks by Dr. Alejandro Diaz
About me (Dr. Alejandro Diaz):
I am a Pediatric Allergist / Immunologist and Global Health Expert with extensive international experience. I have delivered conferences in over 27 countries around the globe on topics of medicine, migration, biosecurity, and related topics. This includes prestigious venues such as the White House, the US Capitol, the Romanian Parliament, the European Parliament in Brussels, the Mexican Senate of the Republic, the United Nations in Geneva, Japanese Parliament, among others.
My career encompasses diverse roles in healthcare including private practice, health systems, and advisory positions for medical service companies, governments, and government entities worldwide.